Check the ingredients!
... live healthy!


![]() Benzoyl Peroxide
Benzoyl Peroxide
Rating : 6
| Evaluation | N. Experts | Evaluation | N. Experts |
|---|---|---|---|
| 1 | 6 | ||
| 2 | 7 | ||
| 3 | 8 | ||
| 4 | 9 | ||
| 5 | 10 |
Pros:
Antibacterial (1) Skin protective (1)0 pts from admin
| Sign up to vote this object, vote his reviews and to contribute to Tiiips.Evaluate | Where is this found? |
| "Descrizione" about Benzoyl Peroxide by admin (19362 pt) | 2024-Apr-17 17:16 |
| Read the full Tiiip | (Send your comment) |
Benzoyl Peroxide is an organic compound primarily used as an acne-fighting agent. It is effective in treating acne by reducing the number of bacteria on the skin, decreasing inflammation, and helping to clear blocked pores. Applied to the skin in the form of a gel or cream, benzoyl peroxide releases oxygen, which kills anaerobic bacteria and promotes skin peeling and cell renewal.
Chemical Industrial Synthesis Process
What it is used for and where
Cosmetics - INCI Functions
Oxidising. This ingredient has the ability to change the chemical nature of another ingredient either by adding oxygen or by removing hydrogen.
Main uses and benefits of benzoyl peroxide.
Safety
It is one of the most common topical treatments for mild to moderate acne, but it can cause dryness, redness, and scaling, particularly during the first few weeks of treatment.
Benzoyl peroxide is considered effective alternative antimicrobial therapy for acne (5).
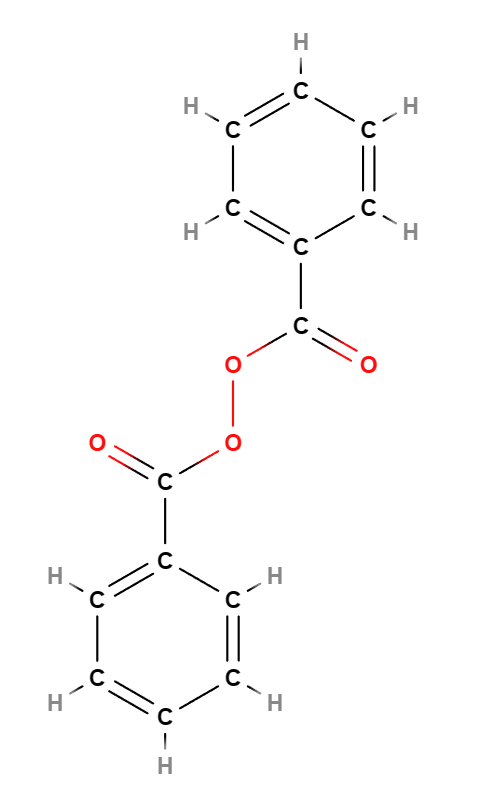 | 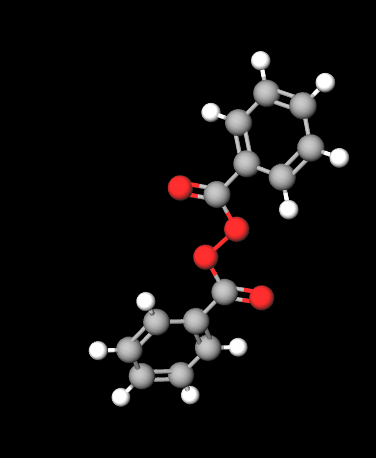 |
Molecular Formula C14H10O4
Molecular Weight 242.23 g/mol
CAS 94-36-0
UNII W9WZN9A0GM
EC Number 202-327-6
DTXSID6024591
Synonyms:
Peroxide, dibenzoyl
Dibenzoyl peroxide
Benzoyl superoxide
Bibliografia_____________________________________________________________________
(1) Kawashima M, Nagare T, Doi M. Clinical efficacy and safety of benzoyl peroxide for acne vulgaris: Comparison between Japanese and Western patients. J Dermatol. 2017 Nov;44(11):1212-1218. doi: 10.1111/1346-8138.13996. Epub 2017 Aug 9. PMID: 28791735; PMCID: PMC5697687.
Abstract. Benzoyl peroxide (BPO) has been well established as a common medication for acne vulgaris in many countries (e.g. in Europe and the USA), where clinical data have been accumulated over a long time. In Japan, the use of BPO for acne treatment was approved in 2014, and the results of clinical trials in Japanese patients have recently been reported. This review compares clinical study results between Japanese and Western patients. Clinical studies that had been performed in Western countries were searched on the basis of the criteria, double-blind studies of BPO monotherapy and comparison with a vehicle group. Two reports of Japanese studies were also selected by using the same criteria. Efficacy was assessed by comparing the mean difference between the BPO and the vehicle groups for reduction rate in the number of lesions from baseline, and there were no differences between Japanese and Western patients. Safety assessment also showed that the incidence of adverse events was higher in Japanese patients than in Western patients, but the characteristics of the adverse events were not different. Therefore, we conclude that there are no significant differences in the efficacy and safety of BPO between these patient populations. The efficacy and safety of long-term use in Japanese patients are also expected to be applicable to those in Western patients.
Stein Gold L, Baldwin H, Kircik LH, Weiss JS, Pariser DM, Callender V, Lain E, Gold M, Beer K, Draelos Z, Sadick N, Pillai R, Bhatt V, Tanghetti EA. Efficacy and Safety of a Fixed-Dose Clindamycin Phosphate 1.2%, Benzoyl Peroxide 3.1%, and Adapalene 0.15% Gel for Moderate-to-Severe Acne: A Randomized Phase II Study of the First Triple-Combination Drug. Am J Clin Dermatol. 2022 Jan;23(1):93-104. doi: 10.1007/s40257-021-00650-3.
(2) Eichenfield DZ, Sprague J, Eichenfield LF. Management of Acne Vulgaris: A Review. JAMA. 2021 Nov 23;326(20):2055-2067. doi: 10.1001/jama.2021.17633.
Abstract. Importance: Acne vulgaris is an inflammatory disease of the pilosebaceous unit of the skin that primarily involves the face and trunk and affects approximately 9% of the population worldwide (approximately 85% of individuals aged 12-24 years, and approximately 50% of patients aged 20-29 years). Acne vulgaris can cause permanent physical scarring, negatively affect quality of life and self-image, and has been associated with increased rates of anxiety, depression, and suicidal ideation. Observations: Acne vulgaris is classified based on patient age, lesion morphology (comedonal, inflammatory, mixed, nodulocystic), distribution (location on face, trunk, or both), and severity (extent, presence or absence of scarring, postinflammatory erythema, or hyperpigmentation). Although most acne does not require specific medical evaluation, medical workup is sometimes warranted. Topical therapies such as retinoids (eg, tretinoin, adapalene), benzoyl peroxide, azelaic acid, and/or combinations of topical agents are first-line treatments. When prescribed as a single therapy in a randomized trial of 207 patients, treatment with tretinoin 0.025% gel reduced acne lesion counts at 12 weeks by 63% compared with baseline. Combinations of topical agents with systemic agents (oral antibiotics such as doxycycline and minocycline, hormonal therapies such as combination oral contraception [COC] or spironolactone, or isotretinoin) are recommended for more severe disease. In a meta-analysis of 32 randomized clinical trials, COC was associated with reductions in inflammatory lesions by 62%, placebo was associated with a 26% reduction, and oral antibiotics were associated with a 58% reduction at 6-month follow-up. Isotretinoin is approved by the US Food and Drug Administration for treating severe recalcitrant nodular acne but is often used to treat resistant or persistent moderate to severe acne, as well as acne that produces scarring or significant psychosocial distress. Conclusions and relevance: Acne vulgaris affects approximately 9% of the population worldwide and approximately 85% of those aged 12 to 24 years. First-line therapies are topical retinoids, benzoyl peroxide, azelaic acid, or combinations of topicals. For more severe disease, oral antibiotics such as doxycycline or minocycline, hormonal therapies such as combination oral conceptive agents or spironolactone, or isotretinoin are most effective.
(3) Ly S, Kamal K, Manjaly P, Barbieri JS, Mostaghimi A. Treatment of Acne Vulgaris During Pregnancy and Lactation: A Narrative Review. Dermatol Ther (Heidelb). 2023 Jan;13(1):115-130. doi: 10.1007/s13555-022-00854-3.
(4) Titus S, Hodge J. Diagnosis and treatment of acne. Am Fam Physician. 2012 Oct 15;86(8):734-40.
Abstract. Acne is a chronic inflammatory skin disease that is the most common skin disorder in the United States. Therapy targets the four factors responsible for lesion formation: increased sebum production, hyperkeratinization, colonization by Propionibacterium acnes, and the resultant inflammatory reaction. Treatment goals include scar prevention, reduction of psychological morbidity, and resolution of lesions. Grading acne based on lesion type and severity can help guide treatment. Topical retinoids are effective in treating inflammatory and noninflammatory lesions by preventing comedones, reducing existing comedones, and targeting inflammation. Benzoyl peroxide is an over-the-counter bactericidal agent that does not lead to bacterial resistance. Topical and oral antibiotics are effective as monotherapy, but are more effective when combined with topical retinoids. The addition of benzoyl peroxide to antibiotic therapy reduces the risk of bacterial resistance. Oral isotretinoin is approved for the treatment of severe recalcitrant acne and can be safely administered using the iPLEDGE program. After treatment goals are reached, maintenance therapy should be initiated. There is insufficient evidence to recommend the use of laser and light therapies. Referral to a dermatologist should be considered if treatment goals are not met.
(5) Leyden, J. J., Hickman, J. G., Jarratt, M. T., Stewart, D. M., & Levy, S. F. (2001). The efficacy and safety of a combination benzoyl peroxide/clindamycin topical gel compared with benzoyl peroxide alone and a benzoyl peroxide/erythromycin combination product. Journal of Cutaneous Medicine and Surgery: Incorporating Medical and Surgical Dermatology, 5, 37-42.
Abstract. Background: Topical clindamycin and benzoyl peroxide have each demonstrated clinical efficacy in the treatment of acne vulgaris. When used in tandem, they promise greater efficacy than either individual agent through their antibacterial and anti-inflammatory effects. Objective: To determine the efficacy and safety of combination benzoyl peroxide/clindamycin compared with benzoyl peroxide or benzoyl peroxide/erythromycin in the treatment of acne. Methods: In this randomized, 10-week, multicenter, single-blind trial, 492 patients with moderate to moderately severe acne were treated twice daily with 5% benzoyl peroxide/1% clindamycin, 5% benzoyl peroxide, or 5% benzoyl peroxide/3% erythromycin and assessed every 2 weeks. Results: Compared with benzoyl peroxide, benzoyl peroxide/clindamycin demonstrated significantly greater reductions in inflammatory lesions (p = 0.04) and significantly greater overall improvement as assessed by physicians (p ? 0.04) and patients (p <0.001). Benzoyl peroxide/clindamycin demonstrated a nonsignificant trend for greater efficacy compared to benzoyl peroxide/erythromycin. Dry skin was the most frequent (?7.3%) adverse event with all three therapies. Conclusion: Benzoyl peroxide/clindamycin demonstrated improved efficacy and similar tolerability to benzoyl peroxide used alone and was similar to benzoyl peroxide/erythromycin, making this combination product an effective alternative antimicrobial therapy for acne.
| Sign up to vote this object, vote his reviews and to contribute to Tiiips.EvaluateClose | (0 comments) |
Read other Tiiips about this object in __Italiano (1)
Component type: Chemical Main substances: Last update: 2024-04-17 16:48:51 | Chemical Risk: |